2025 Virtual Conference on Pain and Palliative Care
Tuesday, May 20, 2025
11:30am – 5:30pm ET
The eighth annual Virtual Conference with live continuing education on Pain and Palliative Care is hosted online by the Society of Pain & Palliative Care Pharmacists (SPPCP) and accredited by the American Pharmacists Association (APhA).
This year, there will be four live continuing education presentations for a total of 5 hours of continuing education credits and one homestudy course to complete at your convenience for 1 hour of continuing education credit.
This year brings back the fifth annual pre-conference opportunity to share research at the SPPCP Research Forum, including interactive presentations by researchers.
Can’t make the 2025 SPPCP Virtual Conference live? Don’t worry - you can still access all the valuable content! The full conference recording will be available for purchase as well. You can explore all 5 hours of expert-led sessions covering pain, palliative care, and hospice topics at a time convenient for you. The recording will be available for purchase in early June 2025. Please note that there are no continuing education (CE) credits available for the recorded program.
Pharmacists: Sessions approved for continuing pharmacy education credits are indicated by an ACPE number and the number of CEUs. To earn CPE for a session accredited by APhA, participants must attend the entire session, submit an attendance code, complete a session evaluation, and claim credit.
Advanced Practice Nurses: Programs accredited by ACPE are listed by the American Nurses Credentialing Center (ANCC) and the American Association of Nurse Practitioners (AANP) as an acceptable accredited continuing education organizations for required CE, including pharmacology credits, and for applicants seeking renewal through CE credit. Contact your credentialing organization for more information.

Accreditation is provided by The American Pharmacists Association. The American Pharmacists Association is accredited by the Accreditation Council for Pharmacy Education.
Programs are accredited for continuing education through a partnership with the American Pharmacists Association.
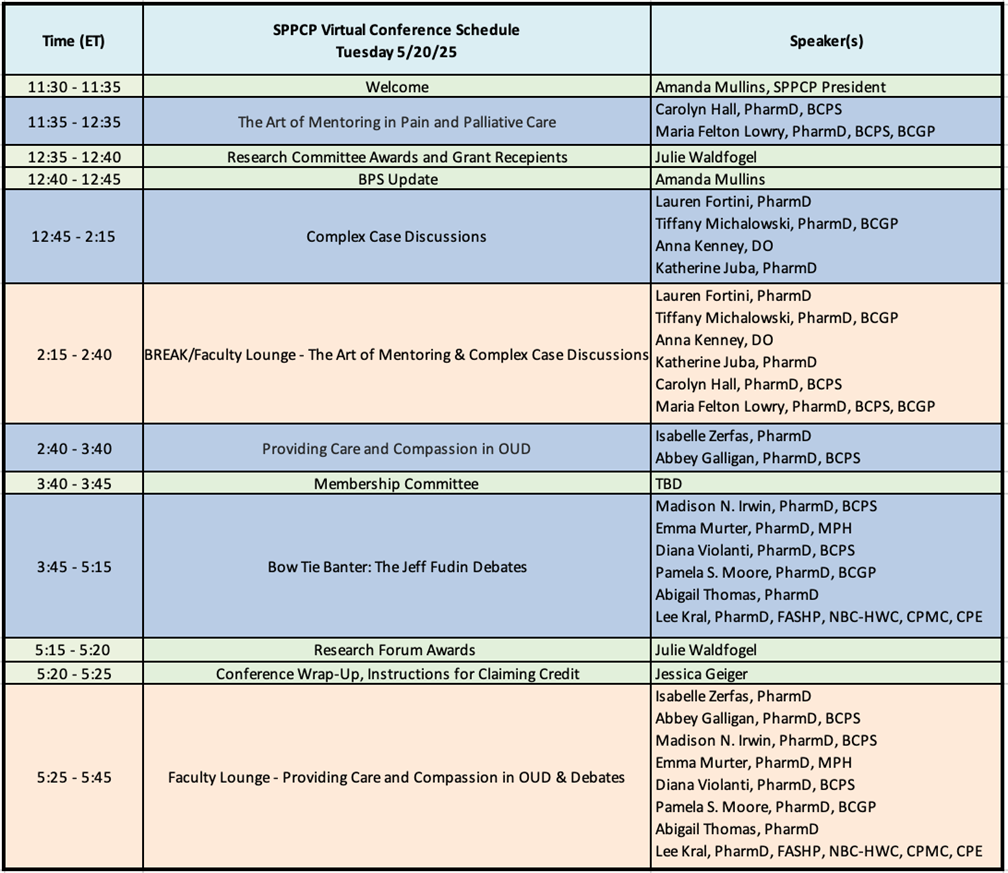
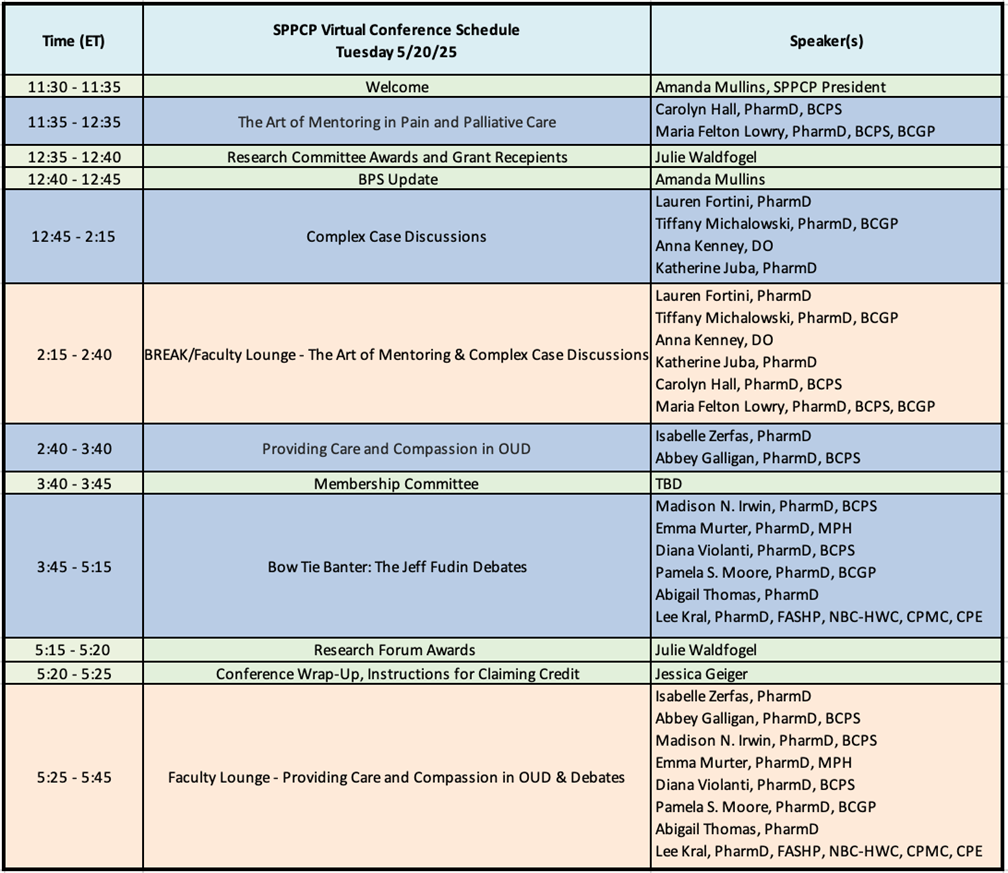
Live Meeting Schedule
2025 VC Program List
- Pain and Progress: Providing Care and Compassion in OUD (1 hour live CE)
- Complex Case Discussions 2025 (1.5 hours live CE)
- The Art of Mentoring in Pain and Palliative Care (1 hour live CE)
- Jeff Fudin Debates 2025 (1.5 hours live CE)
- Low-Dose Naltrexone for Chronic Pain
- Psilocybin for the Management of Mood and Suffering
- The Use of Anticholinergics for Terminal Secretions
- Communication Basics for the Palliative Pharmacist (1 hour homestudy CE)
Presentation Faculty, Descriptions, and Learning Objectives
| Title: |
The Art of Mentoring in Pain and Palliative Care |
| Faculty: |
Carolyn Hall, PharmD, BCPS
Maria Felton Lowry, PharmD, BCPS, BCGP |
| CE Credits: |
1 hour live CE |
Course
Description: |
Mentorship plays an essential role in the professional and personal growth of healthcare professionals, particularly in specialized fields like pain management and palliative care. This presentation explores the pivotal role mentors play in shaping practice, advancing clinical expertise, and fostering leadership skills. Attendees will gain insights into the benefits of mentorship, strategies for building successful mentor-mentee relationships, and the impact mentorship has on professional development and practice advancement. The session will also include an interactive component where attendees will create a personal mentor-mentee roadmap. |
Learning
Objectives: |
- Describe the critical role mentors play in fostering professional development and career progression of pain and palliative care pharmacists
- Identify characteristics of effective mentors and strategies for establishing and maintaining successful mentor-mentee relationships.
- Discuss the benefits of mentorship including skill development, leadership growth, and professional networking.
- Recall the process of creating a mentorship roadmap to ensure successful future mentor-mentee relationships.
|
| Title: |
Complex Case Discussions 2025 |
| Faculty: |
Lauren Fortini, PharmD
Tiffany Michalowski, PharmD, BCGP
Anna Kenney, DO; Katherine Juba, PharmD |
| CE Credits: |
1.5 hours live CE |
Course
Description: |
This program will examine real-world cases to address the challenges of managing complex cancer pain. Through patient case discussions, participants will explore evidence-based treatment strategies, including the role of lidocaine infusions, approaches to severe bone pain, and the importance of shared decision-making. By integrating clinical expertise with patient-centered care, this session will equip providers with practical tools to optimize pain management in complex cancer pain. |
Learning
Objectives: |
-
Outline a plan for lidocaine infusion management and discharge medication options for patients who benefit from a lidocaine infusion.
-
Utilize a patient case to highlight the importance of shared decision-making, balancing goals of care, and interprofessional collaboration when caring for a patient with complex cancer pain.
-
Summarize options for management of severe bone pain secondary to Acute Myeloid Leukemia, including disease-state specific risks for consideration
|
| Title: |
Pain and Progress: Providing Care and Compassion in OUD |
| Faculty: |
Isabelle Zerfas, PharmD
Abbey Galligan, PharmD, BCPS |
| CE Credits: |
1 hour live CE |
Course
Description: |
This program will include defining opioid use disorder, pathophysiology of opioid use disorder, and medical management of opioid use disorder. Medical management will include a review of the initiation and management of primarily buprenorphine, but also discussion of methadone, and naltrexone. Pharmacology of these agents will also be briefly reviewed. Management of acute and chronic pain in the context of opioid use disorder, including perioperative pain management in this context will be covered. |
Learning
Objectives: |
- Recognize features opioid use disorder compared to other facets of opioid dependence and identify basic management strategies for varying degrees of opioid dependence
- Recall pharmacologic management strategies for opioid use disorder
- Identify strategies for acute pain management in the setting of opioid use disorder
|
| Title: |
Bowtie Banter: Jeff Fudin Debates 2025 |
| Faculty: |
Madison N. Irwin, PharmD, BCPS
Emma Murter, PharmD, MPH
Diana Violanti, PharmD, BCPS
Pamela S. Moore, PharmD, BCGP
Abigail Thomas, PharmD
Lee Kral, PharmD, FASHP, NBC-HWC, CPMC, CPE
|
| CE Credits: |
1.5 hours live CE |
Course
Description: |
The Jeff Fudin Debates carry on a long-standing tradition of clinical debates in pain and palliative care. There are many controversial topics in this area of practice, and these debates will delve into the evidence on both sides of each topic. The issues debated will focus on pain management, palliative care, and hospice topics of interest to healthcare practitioners who care for these patients. Debates this year will include the use of low-dose naltrexone in chronic pain, psilocybin-assisted therapy in the management of mood and suffering, and the use of anticholinergics for terminal secretions. |
Learning
Objectives: |
- Recognize the pros and cons of the use of low dose naltrexone in chronic pain
- Discuss the efficacy and safety of psilocybin-assisted therapy (PAT) in the management of mood and suffering
- Describe the benefits and cautions when considering anticholinergics for terminal secretions
|
| Title: |
Communication Basics for the Palliative Pharmacist |
| Faculty: |
Taylor Butler, PharmD, BCOP, BCPS |
| CE Credits: |
1 hour homestudy CE |
Course
Description: |
Despite patient education commonly being a core job requirement for pharmacists, training in communication skills is lacking. For patients with disease-limiting illnesses who have received bad news, these interactions with patients or family members may be especially challenging during stressful times. The goal of this presentation is to review what is known about stressful conversations and how palliative communication can be beneficial. Techniques to approach and communicate with these patients and their family members will be discussed. At the conclusion of the program, attendees will understand the importance of these techniques and feel confident in applying some of the simple suggestions. |
Learning
Objectives: |
- Recognize the role of a clinical headline in a patient interaction
- Differentiate informational versus emotional states in patient conversations
- Identify areas where new communication techniques can be applied based on patient state and informational needs
|
|